Fill Out Your Maryland Employees Vision Template
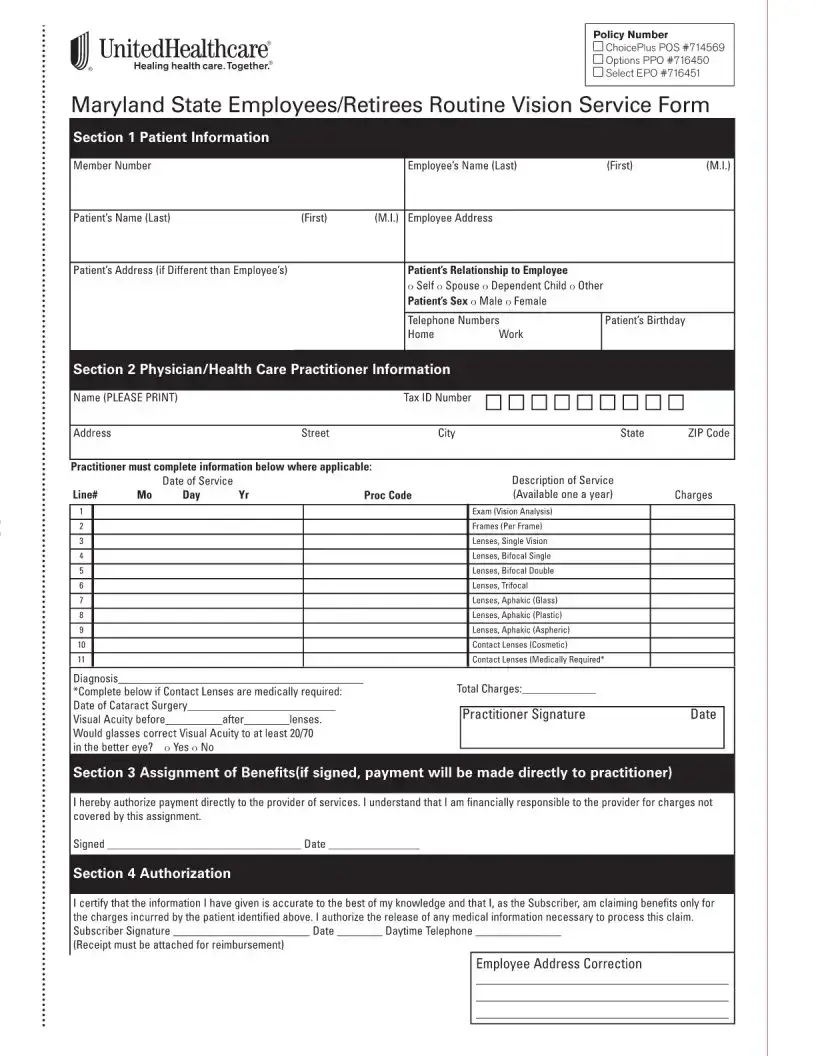
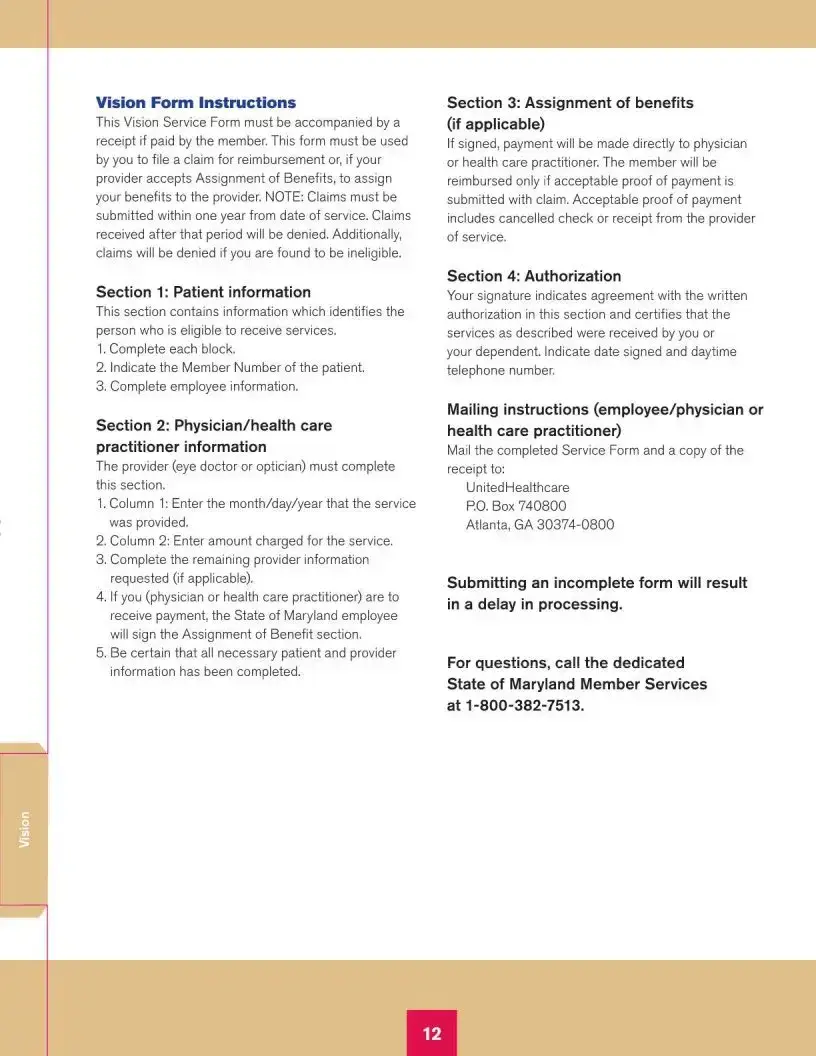
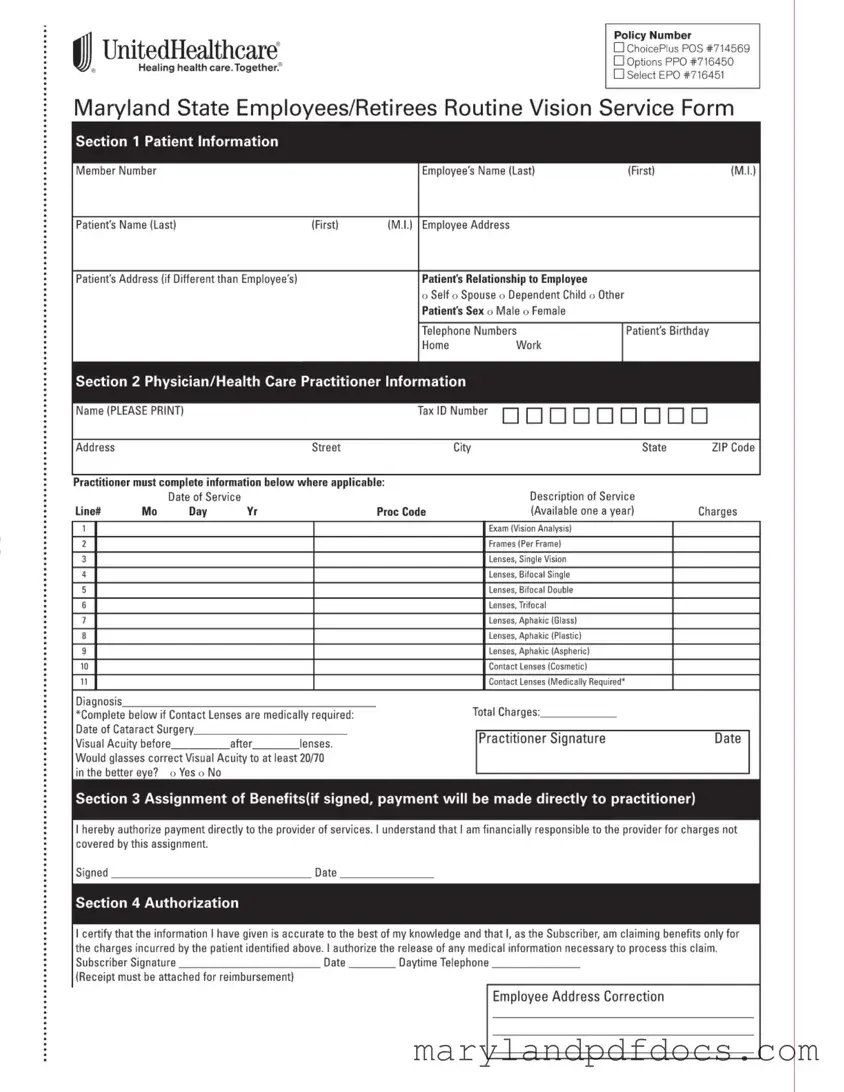
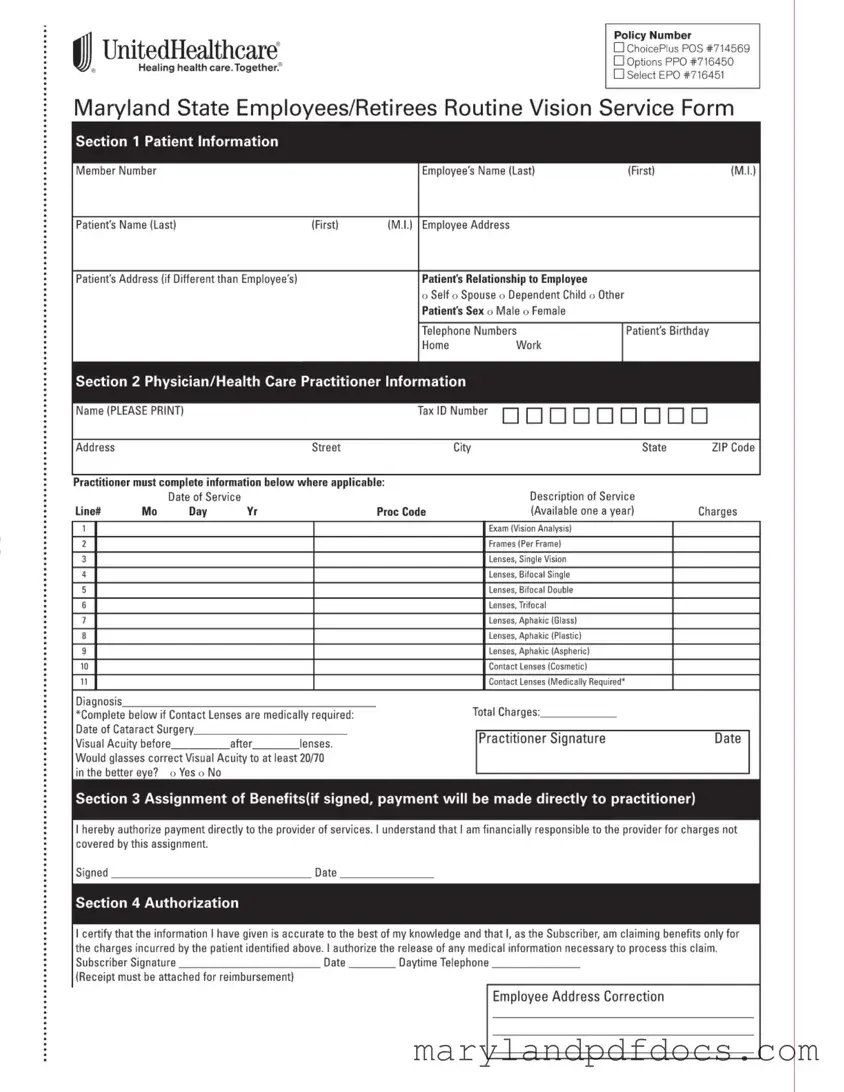
The Maryland Employees Vision Form is a document used by state employees and retirees to claim reimbursement for vision services. This form facilitates the assignment of benefits to healthcare providers, ensuring that eligible individuals receive the necessary eye care without upfront costs. To get started on your claim, fill out the form by clicking the button below.
Launch Maryland Employees Vision Editor
Fill Out Your Maryland Employees Vision Template
Launch Maryland Employees Vision Editor
Launch Maryland Employees Vision Editor
or
Free Maryland Employees Vision PDF
You’ve already started — finish it
Fill out Maryland Employees Vision digitally in just minutes.