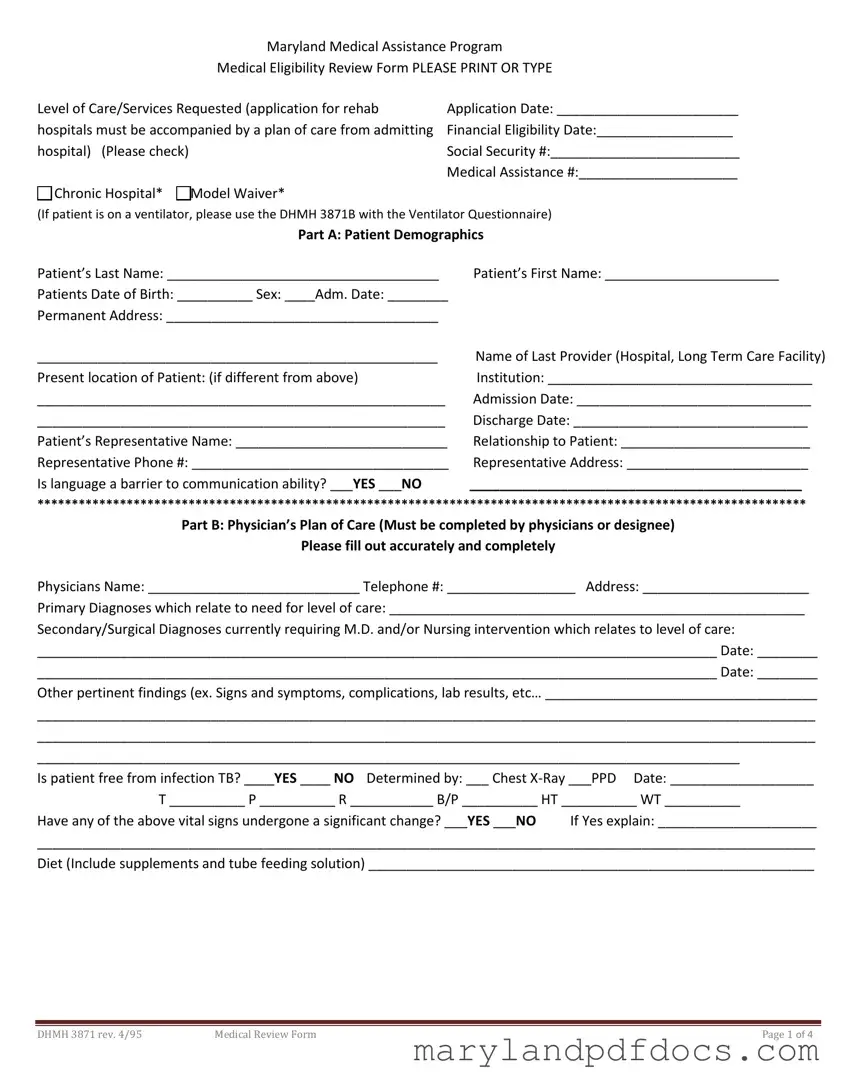
Maryland Medical Assistance Program
Medical Eligibility Review Form PLEASE PRINT OR TYPE
Level of Care/Services Requested (application for rehab |
Application Date: ________________________ |
hospitals must be accompanied by a plan of care from admitting |
Financial Eligibility Date:__________________ |
hospital) (Please check) |
Social Security #:_________________________ |
|
Medical Assistance #:_____________________ |
Chronic Hospital* Model Waiver* |
|
(If patient is on a ventilator, please use the DHMH 3871B with the Ventilator Questionnaire)
Part A: Patient Demographics
Patient’s Last Name: ____________________________________ |
Patient’s First Name: _______________________ |
Patients Date of Birth: __________ Sex: ____Adm. Date: ________ |
|
Permanent Address: ____________________________________ |
|
_____________________________________________________ |
Name of Last Provider (Hospital, Long Term Care Facility) |
Present location of Patient: (if different from above) |
Institution: ___________________________________ |
______________________________________________________ |
Admission Date: _______________________________ |
______________________________________________________ |
Discharge Date: _______________________________ |
Patient’s Representative Name: ____________________________ |
Relationship to Patient: _________________________ |
Representative Phone #: __________________________________ |
Representative Address: ________________________ |
Is language a barrier to communication ability? ___YES ___NO |
____________________________________________ |
****************************************************************************************************************
Part B: Physician’s Plan of Care (Must be completed by physicians or designee)
Please fill out accurately and completely
Physicians Name: ____________________________ Telephone #: _________________ Address: ______________________
Primary Diagnoses which relate to need for level of care: _______________________________________________________
Secondary/Surgical Diagnoses currently requiring M.D. and/or Nursing intervention which relates to level of care:
__________________________________________________________________________________________ Date: ________
__________________________________________________________________________________________ Date: ________
Other pertinent findings (ex. Signs and symptoms, complications, lab results, etc… ____________________________________
_______________________________________________________________________________________________________
_______________________________________________________________________________________________________
_____________________________________________________________________________________________
Is patient free from infection TB? ____YES ____ NO Determined by: ___ Chest X-Ray ___PPD Date: ___________________
T __________ P __________ R ___________ B/P __________ HT __________ WT __________
Have any of the above vital signs undergone a significant change? ___YES ___NO If Yes explain: _____________________
_______________________________________________________________________________________________________
Diet (Include supplements and tube feeding solution) ___________________________________________________________
|
|
|
DHMH 3871 rev. 4/95 |
Medical Review Form |
Page 1 of 4 |
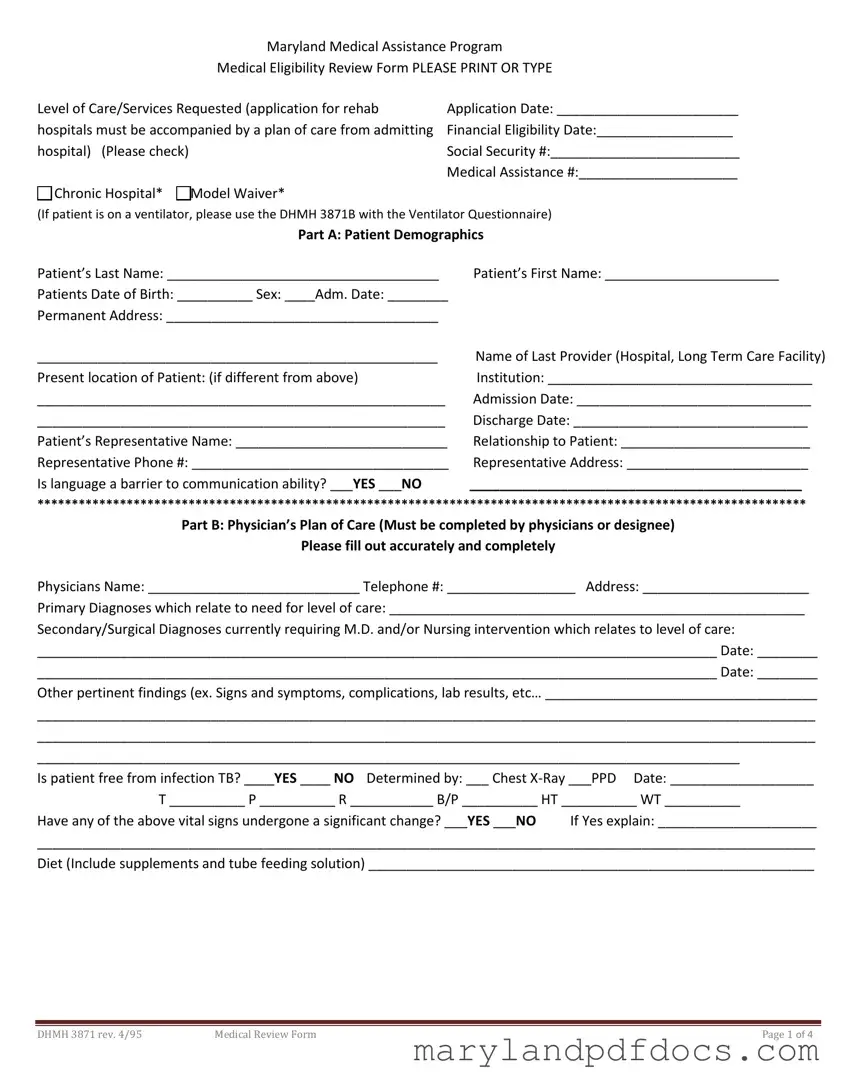
Patient’s Name: ______________________________
Medication which will be continued:
Treatment which will be continued: DescriptionFrequencyDuration if Temporary
____ Ventilator: ____________________________________________________________________________________
____ O2 (as well as sats and frequency): _________________________________________________________________
____ Monitor (apnea/bradycardia (A/B), other: ___________________________________________________________
____ Suctioning: ____________________________________________________________________________________
____ Trach Care: ____________________________________________________________________________________
____ IV Line/fluids (indicate central or peripheral): _________________________________________________________
____ Tube Feeding (specify type of tube): ________________________________________________________________
____ Colostomy/ileostomy care: _______________________________________________________________________
____ Catheter/continence device (specify type): __________________________________________________________
____ Frequent labs related to nutrition/needs (describe): ___________________________________________________
____ Decubitus (include size, location, stage, drainage, and signs of infection, also Tx regimen): _____________________
__________________________________________________________________________________________________
____ Other (specify): ________________________________________________________________________________
__________________________________________________________________________________________________
Have any medications or treatments recently been implemented, discontinued, and/or otherwise changed? Explain:
_______________________________________________________________________________________________________
_______________________________________________________________________________________________
Impairments/devices (check all that apply) ___Speech ___Sight ___Hearing ___Other (specify) ______________________
___Devices/Adaptive Equipment ________________________________________________________________________
Active Therapy |
Plan |
Frequency |
Est. Duration |
Goal |
Physical Therapy
Occupational Therapy
Speech Therapy
Respiratory
Others
|
|
|
DHMH 3871 rev. 4/95 |
Medical Review Form |
Page 2 of 4 |
Patient’s Name: 5674
Rehabilitation Potential: ______________________________________________________________________________
Discharge Plan: _____________________________________________________________________________________
*If requesting a level of care for rehab hospital, please answer the following questions:
1.Preexisting condition related to current physical, behavioral and mental functions and deficits: __________________
__________________________________________________________________________________________________
2.Reason for out-of-state placement (if applicable): ______________________________________________________
Is patient comatose? ___YES ___NO if yes skip parts C through E and go directly to part F.
PLEASE NOTE: For other adults applicants, complete parts C and D, skip E. For applicants under age 21, skip parts C and D, complete E.
*************************************************************************************************
|
Part C: Functional Status (Use one of the following codes) |
|
(If assistive device (e.g., Wheelchair, Walker) used, note functional ability while using device) |
0. |
Little or no difficulty (completely independent |
2. |
Limited physical assistance by caregiver |
|
or setup only is needed |
3. |
Extensive physical assistance by caregiver |
1. |
Supervision/Verbal cuing |
4. |
Total dependence on others |
___ Locomotion (if using adaptive/assistive device, |
___ Dressing |
Specify type): _____________________________ |
___ Bathing |
___ Transfer bed/chair |
___ Eating |
___ Reposition/Bed mobility |
Appetite (Check one): ___ Good ___ Fair ___ Poor |
Other functional limitations (describe) ______________________________________________________________________
Incontinence management (Circle applicable choices in each category) (Note status with toileting program and/or continence device, if applicable)
Bladder |
|
|
Bowel |
|
|
|
|
|
0 |
|
|
0 |
|
|
Complete control-or infrequent stress incontinence |
1 |
|
|
1 |
|
|
Usually continent-accidents once a week or less |
2 |
|
|
2 |
|
|
Occasionally incontinent- accidents 2+ weekly, but not daily |
3 |
|
|
3 |
|
|
Frequently incontinent- accidents daily but some control present |
4 |
|
|
4 |
|
|
Incontinent- Multiple daily accidents |
|
******************************************************************************************************* |
|
|
|
|
|
|
|
Part D: Cognitive/Behavioral Status |
1. Memory/orientation |
Y=Yes |
N=No |
2. Cognitive skills for daily life decision making and safety (Check one) |
Yes |
No |
|
|
|
|
|
|
|
___ |
___ |
Can recall after 5 minutes |
___ |
Independent decisions consistent and reasonable |
___ |
___ |
Knows current season |
___ |
Modified/some difficulty in new situations only |
___ |
___ |
Knows own name |
|
|
___ |
Moderately impaired/decisions requires cues/supervision |
___ |
___ |
Can recall long past events |
___ |
Severely impaired/rarely or never makes decisions |
___ |
___ |
Knows present location |
|
|
___ |
___ |
Knows family/caretaker |
|
|
3. Communication |
|
0- Always |
1-Usually |
2-Sometimes 3-Rarely |
Ability to understand others |
|
_____ |
_____ |
_____ |
____ |
Ability to make self understood |
_____ |
_____ |
_____ |
____ |
Ability to follow simple commands |
_____ |
_____ |
_____ |
____ |
|
|
|
|
|
|
|
|
|
|
|
|
DHMH 3871 rev. 4/95 |
Medical Review Form |
|
|
|
Page 3 of 4 |
Patient’s Name ____________________________________ |
|
|
4. Behavior issues (enter one code from A and B in the appropriate column) |
|
|
A. Frequency |
B. Easily Altered |
|
|
1= Occasionally |
1= Yes |
|
|
2=Often, but not daily |
2= No |
|
|
3= Daily |
|
|
|
|
|
|
|
|
Description of Problem Behaviors |
A |
B |
|
|
|
|
|
|
|
|
|
|
|
|
5.Most recent mini-mental score ___________________________________ Date: __________________________
Previous mini-mental score ______________________________________ Date: __________________________
*******************************************************************************************************
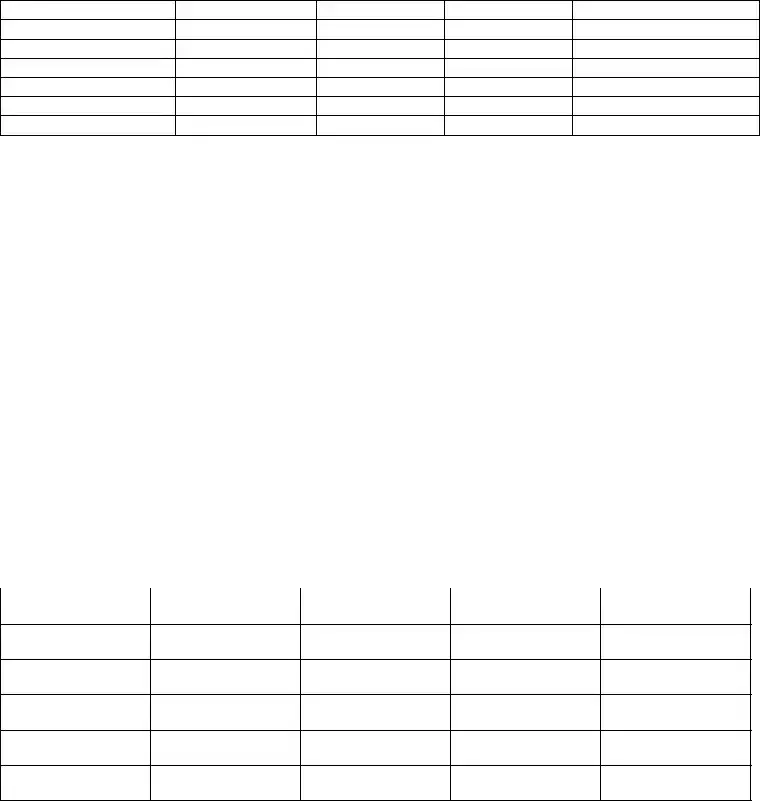
Part E: Functional/Cognitive Status – Pediatric
|
|
Age Appropriate |
|
Functioning Level |
Adaptive Equipment |
|
|
Cognition |
|
|
|
Wheelchair |
|
|
Social Emotional |
|
|
|
Splints/Braces |
|
|
Behavior |
|
|
|
Side Lyer |
|
|
Communications |
|
|
|
Walker |
|
|
Gross Motor Abilities |
|
|
|
Adaptive Seating |
|
|
Fine Motor Abilities |
|
|
|
Communication Devices |
|
|
Feeding |
|
|
|
Other |
|
|
Toileting |
|
|
|
|
|
|
Self Care |
|
|
|
|
|
|
|
Part F: Physician’s Certification for Level of Care |
This patient is certified as in need of the following services (Check One): |
|
|
|
Chronic Hospital |
Model Waiver |
|
|
Other information pertinent to need for Long Term Care: _________________________________________________________
Physician’s Signature: ___________________________________________________________ Date: _____________________
Other than physician completing form: ________________________________________________________________________
SignatureTitlePhoneDate
**********************************************************************************************************
This area is for Agent Determination Only. DO NOT write in this area.
|
|
Renewal |
|
___ Medical Eligibility Established |
MD Advisor ___ |
___Medical Eligibility Established |
MD Advisor___ |
___ Medical Eligibility Denied |
|
___ Medical Eligibility Denied |
|
Effective Date: _____________________ |
Effective Date: _____________________ |
Type of Service: _________________________________ |
Type of Service: __________________________________ |
Certificate Period: From: _____________ To: ___________ |
Certificate Period: From: _____________ To: ___________ |
Agent Signature: _________________________________ |
Agent Signature: __________________________________ |
Date: ___________________________________________ |
Date: ___________________________________________ |
|
|
|
DHMH 3871 rev. 4/95 |
Medical Review Form |
Page 4 of 4 |